Menstrual Cycle
Have you ever wondered why periods come every month, what changes inside your body before and after menstruation, or why your mood and energy levels shift throughout the month? The menstrual cycle is a fascinating biological rhythm that prepares the female body for potential pregnancy and supports reproductive health throughout life.
The cycle is not just about bleeding — it involves hormones, organs, emotions, physical changes, and multiple processes working together in perfect coordination. Understanding the menstrual cycle helps in recognizing what is normal, what may need medical attention, and how to care for reproductive wellbeing.
What is the Menstrual Cycle?
The menstrual cycle is the monthly sequence of hormonal and physical changes that occur in the female reproductive system. It usually begins during puberty and continues until menopause.
The menstrual cycle is important because it:
Supports fertility and reproductive health
Maintains hormone balance
Influences skin, mood, energy, metabolism, and bone health
Helps signal underlying health conditions when irregular
Each cycle begins on the first day of menstruation and ends the day before the next period starts.
How the Menstrual Cycle Works
The menstrual cycle works through a series of hormonal signals between the brain and the reproductive organs.
The brain releases hormones to stimulate the ovaries
An egg begins to mature inside the ovary
The uterus builds a lining to prepare for pregnancy
Ovulation releases the mature egg
If pregnancy does not happen, the lining sheds as menstruation
Hormones that control the menstrual cycle
Estrogen – builds the uterine lining and supports ovulation
Progesterone – stabilizes the lining for pregnancy
FSH (Follicle-Stimulating Hormone) – helps eggs develop
LH (Luteinizing Hormone) – triggers ovulation
Normal menstrual cycle length
A healthy cycle generally lasts 21–35 days. Light variation is normal.
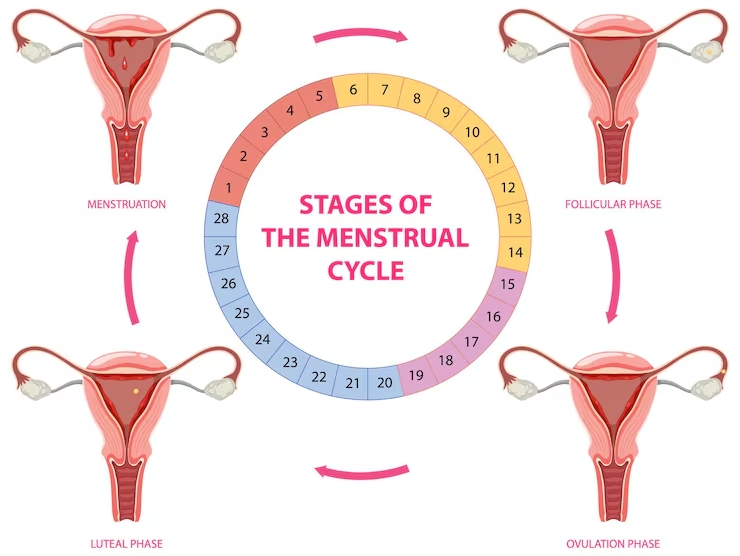
Phases of the Menstrual Cycle
The menstrual cycle has four major phases:
Menstrual Phase
The uterine lining sheds
Bleeding typically lasts 3–7 days
Hormones are low, causing lower energy or cramps in some individuals
Follicular Phase
Begins on the first day of bleeding and continues until ovulation
Estrogen increases, mood and energy often improve
Multiple eggs start developing, but only one fully matures
Ovulation
The mature egg is released from the ovary
This is the most fertile period of the cycle
Some may feel mild pelvic discomfort called ovulation pain
Luteal Phase
Progesterone rises to support potential pregnancy
If pregnancy doesn’t occur, progesterone decreases and the cycle restarts
PMS symptoms may appear due to hormonal shifts
Anatomy Involved in the Menstrual Cycle
Organ | Role |
Ovaries | Store eggs and release one egg during ovulation |
Fallopian Tubes | Carry the egg toward the uterus |
Uterus | Builds a lining for pregnancy and sheds it during periods |
Cervix | Controls flow of menstrual blood; cervical mucus changes through cycle |
Vagina | Passes menstrual blood out of the body |
Endometrium | The lining that thickens and sheds during menstruation |
Menstrual Cycle Changes & Symptoms
Common physical symptoms
Cramps
Bloating
Tender breasts
Fatigue
Back pain
Acne flare-ups
Emotional or mood-related symptoms
Irritability
Sensitivity to stress
Food cravings
Low or high motivation
Normal vs Abnormal variations
Normal | Needs medical attention |
21–35 day cycles | No periods for 90+ days |
3–7 days bleeding | Bleeding longer than 8 days |
Mild cramps | Severe pain affecting daily life |
Clots smaller than a coin | Very large or very frequent clots |
Condition | Description |
Irregular periods | Unpredictable timing |
Dysmenorrhea | Painful cramps |
Heavy menstrual bleeding | Excessive bleeding |
Amenorrhea | No periods for 3+ months |
PMS | Physical + emotional symptoms before periods |
PCOS | Hormonal condition affecting ovulation |
Endometriosis | Tissue similar to uterine lining grows outside uterus |
Doctors may use the following tests when cycle problems occur:
Medical history review
Blood hormone tests
Pelvic ultrasound
Physical examination
Medical & supportive options
Pain relievers (for cramps)
Hormonal medicines (for cycle regulation)
Iron supplements (for heavy bleeding–related anemia)
Lifestyle & nutrition tips
Warm compress for cramps
Regular exercise & stretching
Well-balanced meals
Reducing caffeine & salt during PMS
Hydration
Supplements (only after medical guidance)
Vitamin B6
Magnesium
Omega-3 fatty acids
Iron (if deficiency is present)
Menstrual Hygiene & Self-Care
Good hygiene keeps the menstrual period safe and comfortable.
Change pads/tampons regularly
Try menstrual cups if preferred
Wear breathable underwear
Track your cycle
Rest when the body feels tired
Use heat therapy for cramps
Comfort matters — and listening to your body is the key.
When to Consult a Healthcare Provider
Seek medical help if you experience:
Severe pain interfering with routine
Extremely heavy bleeding
Bleeding between periods
No period for 3+ months (not pregnant)
Sudden cycle change
Fainting, fever, or dizziness during periods
The menstrual cycle is not just a monthly event — it’s a vital sign of reproductive and hormonal health. Every phase of the cycle reflects the body’s natural rhythm. Understanding it empowers women to take charge of both physical and emotional wellbeing.
A healthy lifestyle, good hygiene, and timely medical care ensure a happier and more comfortable menstrual experience. Listening to your body is the greatest form of self-care.